Birth control is not just a means to prevent pregnancy. In fact, birth control can also be used to regulate hormones for people with different medical issues, such as polycystic ovary syndrome or endometriosis. With so many different types of birth control options available, it’s important to understand the differences in their hormonal makeup. Let’s explore the types of birth control hormones and their potential effects on the body. Whether you are looking for a birth control option that fits your lifestyle or a solution to hormonal issues, understanding the differences can help you make an informed decision.
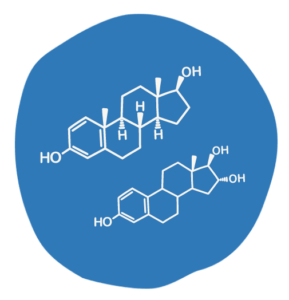
Estrogen and progestin are two hormones commonly used in birth control methods. Estrogen is a hormone that helps prevent ovulation or the release of an egg from the ovary. Progestin, on the other hand, thickens the cervical mucus to prevent sperm from reaching the egg and also makes the uterine lining inhospitable to a fertilized egg, which stops pregnancy.
Various types of birth control methods use estrogen and/or progestin, including progestin-only pills, combined oral contraceptives, the patch, the ring, depot medroxyprogesterone acetate (DMPA), implants, and intrauterine devices (IUDs).
Understanding the differences in hormones and dosages can help individuals make an informed decision about their birth control method. In the following sections, we will explore each commonly used birth control method and its unique hormone combinations in more detail.

Also known as the mini-pill, progestin-only pills are a type of birth control that contain only progestin hormone and no estrogen. They work by thickening the cervical mucus, which makes it more difficult for sperm to reach the egg. These pills must be taken at the same time every day and are highly effective when used correctly.
Unlike combined oral contraceptives, progestin-only pills do not prevent ovulation consistently. This means that while they may prevent ovulation in some women, ovulation may still occur in others. Additionally, progestin-only pills can sometimes cause irregular periods or spotting.
However, they are a good option for women unable to take estrogen, such as those with a history of blood clots or those who are currently breastfeeding/chestfeeding.
Progestin-only pills may interact with certain medications, such as those for treating seizures or HIV. Speaking with your healthcare provider about any potential interactions before starting progestin-only pills is important.
Combined oral contraceptives, also known as “the pill,” are one of the world’s most popular forms of birth control. They contain estrogen and progestin hormones and are taken daily to prevent pregnancy.
Low-dose hormonal birth control pills contain less than 30 micrograms of estrogen. These pills are usually recommended for women sensitive to estrogen’s side effects. Higher-dose pills contain 30 to 50 micrograms of estrogen. The high-dose pills may have more side effects, but they can be more effective in preventing pregnancy.
The hormones in the pill work by preventing ovulation, thickening cervical mucus to prevent sperm from reaching the egg, and thinning the uterine lining to make it harder for a fertilized egg to implant.
While combined oral contraceptives are generally considered safe and effective, they can also come with risks and side effects. These can include nausea, headaches, weight gain, increased risk of blood clots, and stroke risk in certain women.
The patch is another hormonal birth control type that contains estrogen and progestin hormones. It delivers a steady stream of hormones through the skin and into the bloodstream, preventing ovulation.
The patch is typically applied once a week for three weeks, followed by one week without a patch (when you’ll have your period). It’s important to apply the patch to a clean, dry area of skin (like your stomach, upper arm, or butt) and to switch up the location each week to avoid irritation.
Like other hormonal birth control methods, the patch can have potential side effects, including nausea, headaches, mood changes, and changes in sex drive. Some people may also experience skin irritation at the patch site.
It’s worth noting that the patch is not as effective at preventing pregnancy as some other forms of hormonal birth control. It has a failure rate of less than 1% with perfect use, but with typical use, the failure rate increases to about 7%. The patch can still be a convenient and effective option for some people, especially if they struggle with remembering to take a daily pill.
The ring has several benefits. It is over 99% effective when used correctly and can help regulate periods, reduce menstrual cramps, and reduce the risk of ovarian and endometrial cancer.
There are currently two different types of rings on the market. These small, flexible rings are inserted by the user into the vagina, where they release hormones to prevent pregnancy. NuvaRing (the ring is inserted into the vagina and replaced every three weeks) and Annovera (the same ring is inserted into the vagina and removed for a week once a month and used for a year). Both contain a combination of estrogen and progestin hormones, but the specific types and doses of these hormones differ. NuvaRing contains ethinyl estradiol and etonogestrel, while Annovera contains segesterone acetate and ethinyl estradiol.
Ethinyl estradiol is a synthetic form of estrogen, which helps prevent ovulation and thins the uterine lining to reduce the risk of pregnancy. Etonogestrel and segesterone acetate are progestin hormones, which also help prevent ovulation and further thicken the cervical mucus to prevent pregnancy.
Annovera has a lower hormone dose than NuvaRing. This may benefit women sensitive to hormones or experience side effects with higher hormone doses.
The ring can have side effects, including nausea, headaches, and breast tenderness. Additionally, the ring may not be the best option for women sensitive to hormones or with certain medical conditions, such as high blood pressure.
Overall, the vaginal ring is a highly effective method of birth control that provides a convenient and low-maintenance option for many individuals. If you’re considering the ring, be sure to discuss it with your healthcare provider to determine if it’s the right choice for your needs.
![]()
DMPA is a hormonal contraceptive method that involves receiving an injection every three months. It is commonly known as the “birth control shot” or “Depo shot.” DMPA is a progestin-only hormone, meaning that it contains a synthetic form of the hormone progesterone.
The injection works by thickening cervical mucus, which makes it more difficult for sperm to reach the egg. It also suppresses ovulation, so there is no egg to fertilize.
While DMPA is a highly effective form of birth control, some potential side effects exist. These can include irregular periods, weight gain, headaches, and decreased bone density with long-term use. However, it is important to note that not all users will experience these side effects, which can vary greatly from person to person.
DMPA can be a great option for individuals who struggle with remembering to take a daily pill or have medical conditions that make other birth control less safe.
The Implant is a small, flexible rod inserted under the skin of your arm and releases progestin over time. They are an extremely effective form of birth control, with a success rate of over 99%. Implants typically last up to three years but can be removed anytime.
One of the biggest advantages of implants is their convenience – once inserted, you don’t need to think about birth control for three years. Additionally, since they release progestin locally rather than throughout the entire body, they tend to have fewer side effects than other forms of birth control that contain estrogen.
However, like any form of birth control, implants are not perfect. Some people may experience irregular bleeding or spotting, and others may experience side effects such as headaches or acne.
Overall, implants are an excellent option for people looking for long-term, low-maintenance birth control. While they may not be the best choice for everyone, they can be a great option for those looking for effective, reliable contraception without the hassle of remembering to take a pill or use a barrier method every day.
An IUD (intrauterine device) is a small, T-shaped device made of plastic or copper inserted into the uterus to prevent pregnancy. IUDs come in two types: hormonal and non-hormonal.
Hormonal IUDs, such as Mirena and Skyla, release a progestin hormone called levonorgestrel that thickens the cervical mucus to prevent sperm from reaching the egg. The hormone also thins the uterine lining, reducing periods or stopping them altogether. Depending on the type, hormonal IUDs can be effective for up to 8 years.
A non-hormonal IUD, named the Paragard (Copper IUD), is wrapped with a thin layer of copper coil. This creates an inflammatory response in the uterus that is toxic to sperm. Non-hormonal IUDs can be effective for up to 10+ years.
IUDs are one of the most effective forms of birth control and have a low failure rate. They also have the advantage of being a long-term solution for contraception.
If you live or attend school in our service area and are interested in an IUD, Implant, or birth control pills. Call us at 423-265-7837 to schedule an appointment for free birth control. If you have any other questions, please email us at healtheducators@astepaheadchattanooga.org
© A Step Ahead Chattanooga 2024 and website designed by Brightside Creates.
We collect cookies to analyze our website traffic and performance; we never share any personal data. View our Privacy Policy.